The cause of malaria, Malaria in humans is caused by four species of Plasmodium, namely Plasmodium vivax, Pl. falciparum, Pl. malariae and Pl. ovale. Types of malaria caused by four type is of the plasmodium malaria cause different patterns of fever or symptoms of clinical symptoms thereof.
Vivax malaria causing Plasmodium vivax, also called benign tertian malaria (benign), being Pl. falciparum causing malaria falciparum malaria tertian or malignant (malignant). Additionally Pl. falciparum malaria also poses perniciosa and Blackwater Fever. PI. malariae cause malaria malariae, and PI. Ovale cause ovale malaria.
Morphological Plasmodium
In the cells of the liver parenchyma, plasmodium is obtained in the form schizonts preeritrositik that for every species of Plasmodium different sizes and number of merozoites in it. Preeritrositik schizonts shape has never been found in Pl. malariae.
Trofozoit. Trofozoit shape plasmadium distinguished young trofozoit and trofozoit further. In Pl. vivax, trophozoite ring-shaped and contain spots basophils, alu-shaped trofozoit amuboid containing spots Schuffner (Schuffner dots). Infected erythrocytes appear enlarged. In trofozoit Further, it appears the pigment parasites, and often more than one parasite inside the erythrocytes (double infection).
In Pl. falciparum, a young ring-shaped trophozoites looked nucleated and cytoplasmic portion is located on the edge and enitrosit (accole or applique form). Often encountered more than one parasite infection with double chromatin spots. Trofozoit further on this species contains spots Maurer (Maurer dots).
PI. malariae has a young trophozoite ring-shaped, with infected erythrocytes are not enlarged. Further trofozoit ribbon-shaped (band-form) and not found Schuffner spots.
Morphology trofozoit Pl. ovale like trofozoit Pl. vivax, there Schuffner and pigment spots. Infected erythrocytes increase in size, with irregular shapes and jagged, which is typical of this species.
Schizonts. Each species of Plasmodium schizonts have different sizes and the number and arrangement of merozoitnya. At PI. vivax, irregular schizont form, measuring between 9-10 microns and filled erythrocytes appear enlarged. The composition of the merozoites look irregular. In Pl. falciparum, schizonts which measured about 5 microns containing merozoites irregular arrangement. Plasmodium-infected erythrocytes are not enlarged in size.
Schizonts Pl. malariae size of about 7 microns, regular-shaped and filled the infected erythrocytes. Merozoites were 8 pieces, arranged like a rose (rosette shape).
Pl. ovale schizonts have 6 micron sized, filling three-quarters of part of erythrocytes were slightly enlarged. Merozoites number eight, with an irregular arrangement.
Gametocytes. At PI. vivax gametocytes oval or round shape, with red cells increase in size, and contains spots Schuffner. At PI. falciparum, gametocytes shape typical of such bananas with a length of gametocytes larger and the diameter of erythrocytes. PI gametocytes. malariae are round or oval with erythrocytes are not enlarged. Schuffner spots found on infected erythrocytes gametocytes Pl. ovale oval shape. Erythrocytes of normal size, slightly enlarged, or as large as the size of the gametocytes.
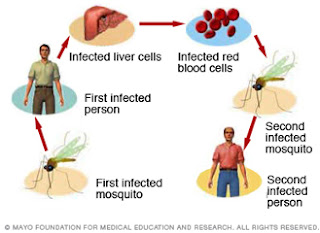
Transmission of malaria, transmission of malaria sporozoites occurs through the bite of a female Anopheles mosquito, the species differ according to geography. Transmission of the asexual forms (trophozoites) causing trophozoite-induced malaria, which can be via blood transfusion (transfusion malaria), via syringe or transmitted from mother to unborn baby melaiui piasen (congenital malaria).
Epidemics of malaria, Malaria is widespread in seiuruh world, either in tropical, temperate and cold climates. To determine the level of malaria endemicity in an area, it must be examined spleen index (spleen index, SI), and the index of parasites (parasite index, PI). In addition it should be investigated to determine the Anopheles mosquito infection rate (infection rate) and the density of mosquitoes (mosquito density). Besides tu socio-cultural life of the population and the environment endemic areas should be studied carefully.
The degree of endemicity of malaria. According to the World Heal Organization (WHO), based on the index override malaria areas are classified into four levels, namely:
Hipoendemis: override index between O to 10 percent;
Mesoendemis: index between li replace up to 50 percent;
Hiperendemis: seialu spleen index above 75 percent with a high index of spleen in adults
Holoendemis: indexes replace always above 75 percent by the spleen index in adults is low. This indicates a strong tolerance of adults against malaria.
Various factors affect the epidemiology of malaria that is the source of infection, either the patient or gametocytes career, namely their capability of transmitting Anopheles mosquito, and sensitive human presence. In endemic areas, especially people with children are the most important source of infection.
Anopheles mosquitoes factors to be considered are the breeding grounds for mosquitoes (breeding places), mosquito longevity and effectiveness in acting as a vector Anopheles transmitters, as well as a dose of sporozoites inoculated each time to suck the blood of patients in both donor and recipient.
The clinical symptoms of malaria, malaria incubation period for each type is different. In malaria vivax and ovale malaria incubation lasts between 10 to 17 days, the falciparum malaria between 8 to 12 days and at malariae malaria, the incubation period lasts between 21 and 40 days.
Malaria show typical symptoms, namely:
Recurrent fever which consists of three stages: freezing (rigor) which lasts between 20 minutes to 1 hour, body heat stage (l-4 hours) and stage sweating a lot (2-3 hours). Splenomegaly and anemia accompanied by malaise.
The pattern of malaria fever. Cycle fever occurs in accordance with the time of skizogeni erythrocytic on each species of Plasmodium.
In tertian malaria, whether malignant or benign, fever takes place every 3rd day (48 hour cycle) and on malariae malaria, fever occurs every 4th day (72 hour cycle). 24-hour cycles of fever can occur if there is a second-generation maturation Pl. vivax within 2 days (called tertian duplex), or third-generation maturation Pl. malariae within 3 days (called kuartana triplex).
A variety of symptoms and complaints of patients can follow the stages of fever, for example, on the stage of rigor, patient shivering despite the patient's body temperature above normal. In stage heat becomes dry skin sufferers, people with red faces and pulse rate increased. Patients also complained of dizziness, nausea, and sometimes vomiting. In children, high fever can cause seizures. At the stadium sweating due to excessive discharge, the patient feels very tired and weak.
Anemia in malaria. Due to rupture of erythrocytes repeatedly during the segmentation process parasites in erythrocytes, patients experience anemia hypochromic microcytic or normocytic hypochromic anemia.
Enlargement of the spleen. One of the important symptoms of malaria are splenomegaly occur after the patient has experienced several bouts of fever. Palpable spleen usually start the second week since the first fever. In the primary malaria, enlarged spleen is unclear and difficult to determine magnifying. The size of an enlarged spleen is important in determining the degree of a malaria endemic area.
Diagnosis of malaria, malaria diagnosis must be determined if found parasites. Examination of peripheral blood is easy to do though sometimes Plasmodium elusive.
Microscopic examination is done with thick drops (thick smear) or with a blood smear (thin-smear). Thick drops performed to determine the rapid diagnosis of malaria, but is undetermined species of the Plasmodium parasite. Blood smear can be used to determine the species of the parasite that causes malaria.
To help with the diagnosis of malaria, especially the concentration of parasites in the blood is very low, performed on peripheral blood serology, for example precipitins test and complement fixation test.
Blood tests also showed a picture of patients decreased hemoglobin, abnormal or decreased leukocytes, platelets decreased, aspartate amino transferase increased, alanine amino transferase increases and increased bilirubin.
Treatment of malaria, anti malaria medication, anti-malaria medicine can be grouped into two groups, namely natural alkaloids, such as quinine and synthetic antimalarial.
Synthetic anti malaria drug is 9-aminoakridin (mepakrin) eg atabrin, kuinakrin, 4-aminokuinoiin (kiorokuin, amodiaquine), 8-aminokuinolin (pamakuin, primaquine), biguanide (proguanil, klopoguanil) and pyrimidine (pyrimethamine). Drug for malaria treatment, Anti malaria drugs can be administered in the form of a combination of pyrimethamine and sulfadoxine are marketed as Fansidar.
Quinine. This natural alkaloid can be administered together with makuin to treat relapsing malaria, acute and severe malaria (given intravenously) or to treat falciparum malaria which is resistant to chloroquine.
Immunity (resistance) to anti malaria drugs. One of the obstacles in combating and controlling malaria is the malaria parasite immunity against anti-malaria drug are used.
A species is declared Plasmodfum still susceptible (sensitive) against certain anti-malarial drugs, if within 7 days of treatment, parasitemi asexual forms had disappeared without a subsequent recurrence (rekrudesensj). This parasite is still sensitive Sensitive stated.
If there has been a parasite resistance to anti-malaria drugs, the malaria drugs should be immediately replaced with other anti-malarial drugs, while malaria control is done by increasing the eradication of malaria vectors are Anopheles mosquitoes.
Prevention of malaria made to the individual and society, namely:
Treat people and people who are sensitive, who resided in endemic areas.
Treating malaria using primaquine career, being able to eradicate gametocytes. However, use of these drugs should not be done en masse because they have side effects.
Preventive treatment in people who will go to malaria-endemic areas
Eradicate the mosquito Anopheles vectors of vector by using appropriate insecticides and destroy the nests of the Anopheles mosquito.
Refrain from mosquito bites by using mosquito nets when sleeping, or using repellen are rubbed on the skin of the body the evening if you're outside the house at night.
Malaria pernicious, pernicious malaria (pernicious malaria) is a collection of symptoms that result from the treatment of falciparum malaria that is not perfect, so the cause of death of patients within one to three days after treatment.
Kanagiutinasi causing any parasite Plasmodium falciparum infected erythrocytes so that the capillaries of various organs unstoppable. This is due to the parasite erythrocytic skizogoni process occurs in the capillary blood vessel organ. The result is a parasitic emboli that are not able to pass through capillaries. Also forms trofozoit and sexual forms of the parasite is attached to each other and also attached to the capillary wall. In pernicious malaria always happen parasitemi weight, either a ring shape or form schizonts.
There are three clinical forms of pernicious malaria, namely cerebral malaria, algid malaria and malaria septikemik.
Cerebral malaria occurs due to brain disorder that causes symptoms of hyperpyrexia, paralysis and coma. In aigid malaria, due to peripheral circulatory failure, patients experience symptoms of collapse with clammy skin. In algid malaria-type gastric collapse accompanied by vomiting, diarrhea koleraik type, and dysentery on the type disenterik.
Septikemik malaria symptoms are the body heat is always high, accompanied by symptoms of pneumonia and cardiac syncope.
Blackwater Fever, Blackwater fever is a form of malaria faiciparum accompanied intravascular hemolysis, fever, and hemoglobinuria.
Blackwater fever is common in patients with malaria faiciparum with the state:
1. Do not have immunity to malaria (non-immune) who received treatment with low doses of quinine.
2. deficiency of glucose-6-phosphate dehydrogenase, so prone to hemolysis of erythrocytes.
In addition, factors low temperatures, fatigue, trauma, pregnant women, childbirth and radiation to the spleen may have an effect on the incidence of blackwater fever.
Pathogenesis Biackwater Fever, a result of the occurrence of intravascular hemolysis, occurs themalbuminemia, hyperbilirubinemia and hemoglobinuria.
Various organ changes, namely:
1. The kidneys become enlarged and dark due to the damming and pigmentation,
2. The liver is enlarged, softened and yellow due to the formation hemosidenin,
3. The gall bladder bile filled with dense dark green,
4. The spleen is enlarged, black for their pigment hemozoin,
5. Hemosidenin many accumulate in the liver, spleen and kidneys.
In times of crisis hemolytic, parasites not found in the blood because it participates destroyed by the process of hemolysis. One week after the crisis ends hemolysis, the parasite can be found in the peripheral blood of patients.
Blackwater Fever diagnosis, blood tests showed normocytic anemia patients with red blood cell count less and 2 million per milliliter, and the hemoglobin is less than 10. During the healing period, it appears the reticulocytosis and lekositosis netrofilik. Biochemical showed increased blood urea, while decreasing cholesterol and greatly decreased haptoglobin.
Complications blackwater fever, blackwater fever Three major complications are renal physiology failure (uremia), liver function failure and circulatory collapse. Blackwater fever death rate of about 20 to 25 percent, mainly due to kidney failure.
Treatment of Blackwater Fever, blackwater fever Every patient should get plenty of rest. Fluid balance must be kept going alkalosis and edema. If needed, brine, parenteral plasma or blood transfusions can be given the appropriate circumstances of the patient. In case of sudden kidney failure, peritoneal dialysis can be given, and in case of hemolytic crisis, give corticosteroids.
Drugs to treat malaria, Anti malaria drug should be administered with caution. Kiorokuin, pyrimethamine or proguanil may be given, but primaquine, kuinakrin, and quinine is contraindicated.

0 Comment
Markup